Hippocrates, famous for the Hippocratic Oath, urged doctors “namely to do good or to do no harm.” This admonition—routinely paraphrased as “first do no harm”—is also a good adage for medical device manufacturers to keep in mind, as the practice of medicine relies more than ever on the devices they make. But while most medical device manufacturers are careful to ensure that their products are safe and reliable, they don’t always give medical device packaging the same careful attention.
That oversight can have serious, even fatal, consequences.
7 Common Mistakes in Medical Device Packaging
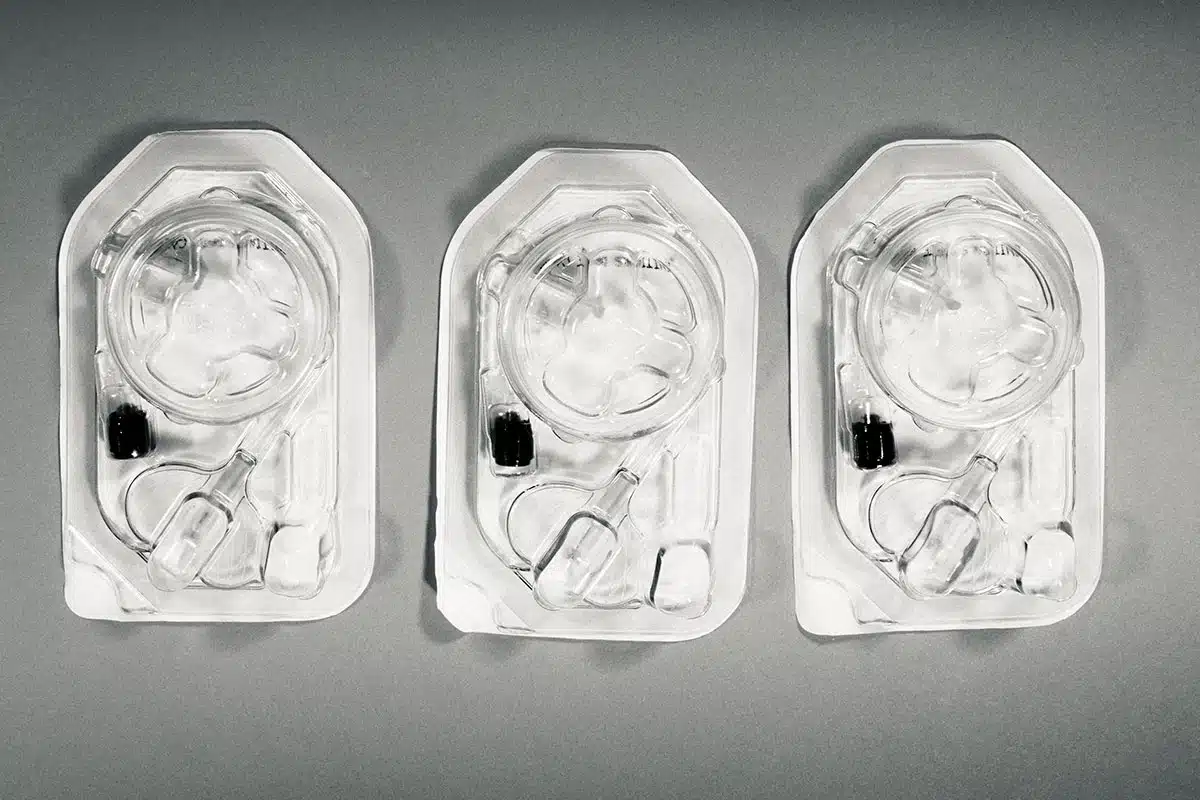
There are two main purposes for medical device packaging: protecting a product so that it arrives intact and in good working order, and maintaining a sterile environment. Contamination is an especially urgent concern. According to the U.S. National Library of Medicine, viral and bacterial infections are among the ten leading causes of morbidity and mortality in the United States.
One way to prevent contamination—and the subsequent recall—of medical devices is with reliable, high-performance packaging. According to the U.S. Food and Drug Administration (FDA), packaging and labeling issues account for 13% of all medical device recalls, which is why some experts assert that medical device packaging is nearly as important as the device itself.
According to the U.S. Food and Drug Administration (FDA), packaging and labeling issues account for 13% of all medical device recalls, which is why some experts assert that medical device packaging is nearly as important as the device itself.
Mistake #1: Losing Sterile Integrity
Ensuring the sterility of medical devices is critical for reducing infection, yet it is the most common defect found in medical device packaging. Unfortunately, some medical device manufacturers fail to create a truly sterile barrier system (SBS) in which to encase their products for transport. This means that in some cases, when their products arrive at the point of use, they fail to meet the aseptic standards required by FDA and International Organization for Standardization (ISO) regulations.
While nonsterile packaging can be the result of contamination at the packaging site, often the issue is more fundamental—the design of the packaging itself. It’s important to keep in mind that packaging can only be made sterile on the inside. A package’s exterior will always arrive at its destination in a nonsterile state. This means it’s essential to design packaging that can be opened without introducing contamination.
So, how can you design your package to limit contamination? The National Library of Medicine found that pouches that had outward-curling seals had significantly lower contamination rates. In other words, if the exterior of a package curled away from the interior as the package was opened, it was far less likely that the outside of the package (the nonsterile surface) would come in contact with the interior’s sterile contents.
Mistake #2: Not Accounting for the Device’s Entire Journey
A sterile barrier system is only useful if it stays intact for its entire journey, which is why your package design must include protective material to shield the SBS from the time of assembly to the point of use. Many sterile packages are damaged due to pinholes, slits, cuts, and tears. To avoid these outcomes, wise manufacturers design an entire packaging system that protects the device—and its SBS—throughout the journey from factory to hospital. This means designing resilient packaging that can withstand exposure to road vibration during long hours of transportation. Packaging must also be strong enough to survive warehouse mishaps like a fall to the ground.
Mistake #3: Ignoring Best Practices for Medical Device Packaging
Whether you’re shipping something as simple as a box of bandages or as complex and delicate as a tracheotome, your packaging is critical. Both the United States and Europe have stringent regulations for medical device packaging. Yet not all manufacturers adhere to best practices and regulations when it comes to certain aspects of their product packaging.
Some manufacturers, for example, fail to get their medical device packaging properly validated. It’s true that validation is an extensive and at times complex process. But the regulations serve a purpose. Rigorously testing your proposed packaging will ensure that it provides an effective barrier against microbial ingress, moisture, and environmental contaminants. Furthermore, a good validation process does more than ensure your packaging meets regulatory requirements. It also guarantees that your device gets to your customer in sterile condition, able to perform as advertised right out of the box. This preserves your brand reputation, and eliminates liability headaches as well.
Of course, your efforts to comply with FDA and ISO regulations can be negated if your product is contaminated by a vendor. So, if you’re working with third-party contractors, be sure to screen them carefully to ensure they’re also adhering to best practices for medical device packaging and shipping.
Mistake #4: Using the Wrong Packaging Material
Many medical devices are packaged using thermoform trays—plastic trays that are made by heating plastic sheets and molding them into the desired tray shape. But there is a wide range of plastic available for this purpose, and choosing the wrong one can lead to packaging failure. For example, if you’re packaging a medical device with a lot of mass, you might need a high-impact plastic such as polycarbonate to reduce fracturing during distribution and handling.
The design of the thermoform tray is also critical. The tray or case must be tight enough to hold the medical device firmly in place. Otherwise, a loose product could jettison through the tray lid and fracture the plastic casing from the inside out. Conversely, packaging must have a bit of give, so that it doesn’t damage sensitive sensors or other high-tech components. A good package design strikes the right balance between these two extremes.
Mistake #5: Using the Wrong Container
In addition to using the right packaging material, you need to choose the right size and strength for your exterior shipping box. For example, if you are using an outer carton to protect your sterile pouch, you need to avoid squeezing the pouch into a too-small carton. You should choose a container that avoids any folding, wrinkling, or creasing of the ends of your sterile pouch. Otherwise, the vibrations of a moving truck could lead to pinholes at the junctures of the creases or folds of the pouch. Complex pouch folds are even more problematic, as they form a concentrated point of stress at the juncture of the materials.
When it comes to the sterile pouches themselves, however, bigger isn’t always better. Some research has found that increased contamination rates are associated with larger pouches versus smaller ones. Unfortunately, the reason for this is not entirely clear. One theory is that larger pouches require more hands-on repositioning to open, and that this increased handling offers more opportunities for contamination.

Mistake #6: Inadequate Testing
Just as it’s important to test and inspect your product, you need to test the effectiveness of your packaging material—and package design—to ensure that the SBS and the outer carton will protect the device as it travels from assembly to customer to storage.
Testing might reveal, for example, that a single sterile barrier is not sufficient to maintain a sterile environment for a product that might sit in a hospital storeroom for up to a year; instead, a double barrier is needed. Real-time aging testing like this will enable you to see how your medical device packaging holds up under storage conditions in which both temperature and humidity can fluctuate widely, especially over an extended period of time.
But what if you’re trying to beat a competitor to market? Or more importantly, get a life-saving medical device to patients as quickly as possible? That’s where testing via accelerated aging—elevating temperatures to artificially speed up the aging process—can be useful. For example, subjecting a sterile barrier system to 40 days of +55°C temperatures has roughly the same effect as storing the SBS at +23°C for a year. That’s a huge time savings.
There is a caveat, however. Using temperatures that are too high—in the hopes of cutting a few more days off the testing process—can cause a package to melt or warp in a way it never would under real-world conditions, negating the purpose of the test. So, exercise caution when applying accelerated aging techniques. Or work with a laboratory that specializes in testing via accelerated aging.
Mistake #7: Neglecting to Develop a Recall Protocol
In addition to protocols for testing, manufacturers should develop specific protocols in case the need for a recall arises. Such a protocol might involve plans for recall initiation, reporting, execution, and monitoring. Recall protocols are especially important right now, as medical device recalls are on the rise. Between 2012 and 2022, recalls increased by 125%. (And medical device adverse event reports increased by over 500%.)
Having protocols in place means you’ll be better prepared to initiate a voluntary recall, which will do less damage to your business reputation than a forced recall. That was the case for medical manufacturer Nurse Assist, LLC. In November 2023, the company issued a voluntary recall on its saline and other water-based products over concerns of compromised sterility. These included various bottles, spray cans, cups, and syringes. When the recall was initially released in November 2023, no adverse effects had been reported. And while the FDA has since received reports of adverse events, Nurse Assist’s prompt, voluntary action has enabled the company to mute the damage to its brand.
Diligence is Needed in Medical Device Packaging
As healthcare providers continue to prioritize infection reduction, and medical device recalls continue to rise, designing and deploying effective medical device packaging is more important than ever. Avoiding the seven pitfalls outlined here is the first step in making sure that your packaging performs in a way that increases patient safety—and enhances your company’s reputation.